While India tries to get back on its feet from the devastating second wave of COVID-19, the nation find its people grappling with a rare fungal disease, called mucormycosis among recovering or recovered coronavirus patients.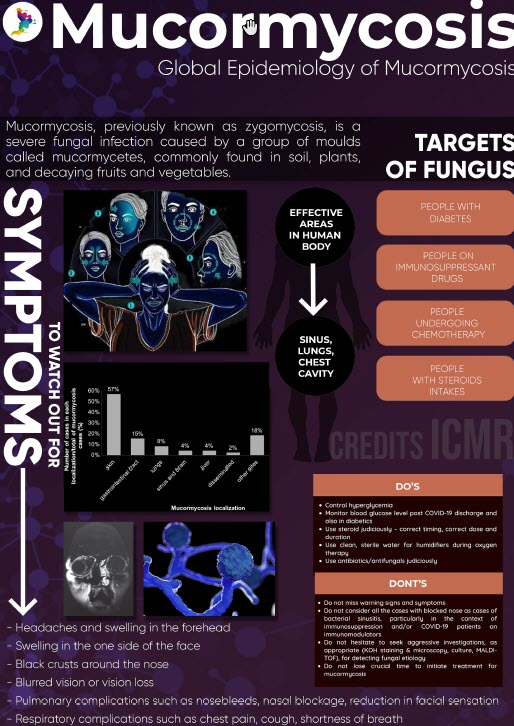 On 20th May, the Ministry of Health and Family Affairs urged all states and union territories to assess the situation and notify mucormycosis as an epidemic under the Epidemic Diseases Act, 1897. The union ministry further mandates all state and private health facilities to report all suspected and confirmed cases of this fungal disorder.
On 20th May, the Ministry of Health and Family Affairs urged all states and union territories to assess the situation and notify mucormycosis as an epidemic under the Epidemic Diseases Act, 1897. The union ministry further mandates all state and private health facilities to report all suspected and confirmed cases of this fungal disorder.
The country has over 11,500 patients suffering with mucormycosis as on May 26. Out of these total cases, nearly 50% are reported from two west Indian states – Gujarat and Maharashtra.
According to experts, an indiscriminate use of steroids in treatment of COVID-19 for immuno-compromised and diabetic patients have led this rare infection into a full fledge epidemic in India.
“The irrational usage of steroids, unhygienic practice of mask wearing, uncontrolled diabetes and improper handling of humidifiers have potentially contributed as major factors for mucormycosis – said Dr. Juzer Sabuwala, a clinical pharmacologist based in Hyderabad. “While steroids are essential medicines, it is a double edged sword, on one hand in COVID management it is a very potent weapon, but if used injudiciously without certified physician consultation, it can predispose patients to secondary infections, one being mucormycosis.” added Dr. Sabuwala.
“However, a proper assessment of cases can offer more scientific answers to all speculation of mucormycosis origination. But this fungus spread rate is very high and it is observed to quickly reach vital organs, including eyes and sometimes brain.”
The Voices asked Dr. Sabuwala about possible treatment plans for mucormycosis patients. He said – “the only line of treatment is a surgical debridement and usage of anti-fungal drug Amphotericin B for a month. After that a careful assessment is made and a prolonged three-month course of oral anti-fungal drugs is prescribed. Of course, these medication carry side-effects of their own.”
While explaining the disease in detail, Dr. Sabuwala said “Mucormycosis commonly presents in 4-5 different forms- in lungs; in sinus and brain; intestines, skin or the central nervous system. The most common symptom in lung mucormycosis is a high grade fever that does not subside despite introduction of antibiotics. While pain and discoloration of nose are the signs of sinus mucormycosis.”
The Indian Council of Medical Research (ICMR) released evidence based advisory for effective screening, diagnosis and management of mucormycosis earlier this month.
This unanticipated fungal infection brought new challenges for already strained Indian healthcare system like shortage of anti-fungal drugs like Amphoterecin B injections and posaconazole pills. The patients and their family members who are already under mental, physical and financial stress of COVID-19, face another nightmare of this fatal infection.
Union Minister for Chemical & Fertilizers Mr. Sadananda Gowda in a twitter message disclosed state-wide allocation of Amphoterecin B injections but they are not sufficient with growing case counts . On ground, patients face great difficulties in acquiring vials from district or state authorities. While COVID-19 cases appears to fall, many rural belts of India is still struggling to get basic life-saving drugs and others like tocilizumab which are scarce in supply.
As of May 26, India has more than 24 lakhs active coronavirus cases and almost 316,000 official deaths, according to John Hopkins statistics.


1 Comment
A timed intervention. India really need to ramp up the production of essential drugs for the same. Thanks for coming up with this story Hussain. Congratulations